What is Menopause?
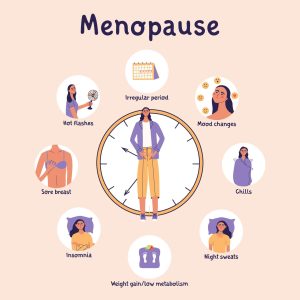
Menopause is a natural biological process that occurs in women typically around their late 40s to early 50s, although it can vary. It marks the end of menstruation and fertility. Menopause is diagnosed after 12 consecutive months without a menstrual period.
During menopause, a woman’s ovaries gradually produce less oestrogen and progesterone, the hormones responsible for regulating the menstrual cycle. This hormonal shift can lead to various physical and emotional symptoms, such as loss of hair, weight gain, hot flashes, night sweats, mood swings, vaginal dryness, and changes in libido.
Menopause is a normal part of aging, but the symptoms can vary widely among women. Some may experience only mild symptoms, while others may find them more severe and disruptive to daily life. However, there are various treatments and lifestyle adjustments that can help manage these symptoms and promote overall well-being during this transitional phase.

What is the difference between Perimenopause and Menopause?
Very Simply put perimenopause is the transitional phase leading up to menopause, characterized by irregular menstrual cycles and fluctuating hormone levels, while menopause itself is the point at which menstruation ceases permanently.
Perimenopause and menopause are both stages in a woman’s life cycle, but they refer to different phases within that cycle:
Perimenopause: This is the transitional phase leading up to menopause. It usually starts several years before menopause, although the exact timing can vary for each woman. During perimenopause, hormone levels, particularly oestrogen, begin to fluctuate irregularly, leading to changes in the menstrual cycle and various physical and emotional symptoms. In the Perimenopause Phase Women may still have menstrual periods during perimenopause, but they may become irregular in frequency and flow.
Menopause: Menopause is the point at which a woman has not had a menstrual period for 12 consecutive months. It marks the end of the reproductive years and the cessation of menstruation. The physical and emotional symptoms seen in perimenopause can remain or fluctuate in menopause. These symptoms usually last for few years post menopause and decrease in intensity and frequency.
How physical therapy can help you
Physiotherapy can play a valuable role in managing symptoms associated with menopause and promoting overall well-being during this transitional phase. While physiotherapy may not directly address hormonal changes, it can offer a holistic approach to managing the physical and emotional changes associated with menopause, empowering women to maintain active, healthy lifestyles and optimize their quality of life during this stage of life.
Here are several ways physiotherapy can be beneficial during menopause:
Exercise Prescription: Physiotherapists can design customized exercise programs tailored to the individual needs and preferences of women experiencing menopause. Regular physical activity can help manage weight, maintain bone density, improve cardiovascular health, and reduce the risk of conditions such as osteoporosis and heart disease, which may become more prevalent after menopause.
Strength Training: Strength training exercises can help counteract the loss of muscle mass and bone density that often occurs during menopause. By incorporating resistance exercises into a woman’s exercise routine, physiotherapists can help maintain muscle strength, improve balance, and reduce the risk of falls and fractures.
Pelvic Floor Rehabilitation: Menopause can lead to changes in the pelvic floor muscles, resulting in symptoms such as urinary incontinence and pelvic organ prolapse. Physiotherapists specializing in pelvic health can provide exercises and techniques to strengthen the pelvic floor muscles, improve bladder control, and alleviate symptoms related to pelvic floor dysfunction.
Pain Management: Menopause may be associated with musculoskeletal pain, such as joint stiffness, back pain, and muscle tension. Physiotherapists can employ various techniques, including manual therapy, stretching exercises, and modalities such as heat or cold therapy, to reduce pain and improve mobility.
Posture Correction: Hormonal changes and age-related factors can contribute to changes in posture and body alignment. Physiotherapists can assess posture and provide strategies to improve alignment, strengthen postural muscles, and reduce the risk of musculoskeletal injuries.
Stress Reduction: Menopause can be a stressful time for many women, and stress can exacerbate symptoms such as hot flashes and mood swings. Physiotherapists can teach relaxation techniques, breathing exercises, and mindfulness practices to help manage stress and promote emotional well-being.